What is a portosystemic shunt?
A portosystemic (liver) shunt is a blood vessel anomaly that results in blood from the abdominal organs (small bowel, large bowel, stomach, etc.) being diverted to the heart and bypassing the liver. The condition may be either a birth defect – a congenital portosystemic shunt, or may be acquired – commonly associated with chronic disease of the liver such as cirrhosis (scarring of the liver).

What are the problems associated with blood shunting?
In the normal individual, nutrients and toxins (poisons) that are absorbed from the intestines are cleared from the circulation when they are passed through the liver via the portal vein, which runs from the intestines into the liver. The liver stores some of the food for energy, uses some of it to make proteins and other substances, and processes any toxic chemicals to make them safe. Maintenance of a normal liver is largely determined by the blood flow through the portal vein. The presence of a portosystemic shunt bypasses the normal portal blood flow to the liver, and in congenital cases this results in the development of a small liver (known as hepatic hypoplasia) and the progressive shrinkage of the liver (hepatic atrophy). The progressive build up of toxins in the bloodstream often results in nervous symptoms (so-called hepatic encephalopathy). Additionally, affected individuals lack the necessary substances to give a ready source of energy, resulting in poor or stunted growth.
What are the clinical signs of a portosystemic shunt?
Clinical signs in congenital cases are often seen at a young age and include small stature, poor muscle development, behavioural abnormalities (walking around in circles, disorientation, unresponsiveness, a quiet demeanour, staring into space, pressing of the head against surfaces) and seizures. Other less common signs include excessive drinking or urinating, apparent blindness, diarrhoea and vomiting. In some animals the signs are associated with or aggravated by eating protein. Other animals are diagnosed when they take a longer time than expected to recover from sedation or an anaesthetic (for example, for an elective procedure such as castration or spaying). Some animals with congenital shunts show no signs until they are older, when they may develop bladder and kidney infections, and possibly bladder stones.
How is a liver shunt diagnosed?
A diagnosis of a liver shunt should be suspected in any individual showing the clinical signs described in the previous section. A more specific diagnosis will require blood tests, including the measurement of bile acid or ammonia concentrations. However, a liver shunt cannot be definitively diagnosed by blood tests; shunting can only be found with advanced techniques such as ultrasound scans, specialised X-rays (a portovenogram – see below), CT scanning, MRI scanning, and/or exploratory surgery.
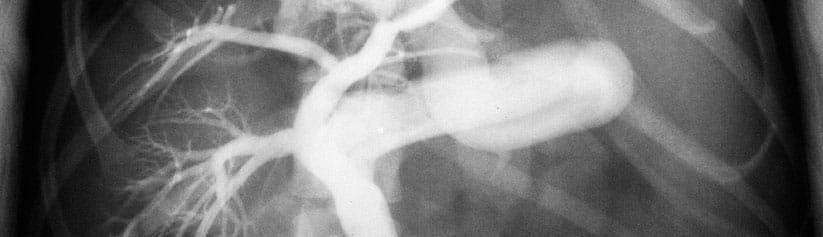
What is a portovenogram?
A portovenogram is an X-ray examination that allows the anatomy of the liver shunt to be very accurately visualised. The procedure is performed under general anaesthesia and requires the surgical opening of the abdomen. A vein draining the small bowel is injected with a dye that shows up on an X-ray (a contrast agent). The X-rays are obtained during the injection of the contrast agent, thereby producing an image of the abnormal liver shunt. Sometimes the X-rays are obtained as moving images; this is called fluoroscopy.
Since the portovenogram requires surgical intervention, it is carried out as part of the surgical investigation and management of the liver shunt. The portovenogram is viewed as the ‘gold standard’ with regard to producing images of any liver shunts or vascular abnormalities. The procedure is considered very safe and without specific complications. It will commonly form part of the management of any case undergoing the investigation and management of a liver shunt.
What does the surgical correction of a liver shunt involve?
The surgical management of portosystemic shunts can be very demanding – this, along with the requirement for specialist equipment such as intra-operative fluoroscopy, means that it is best performed by a specialist soft tissue surgeon working from a well equipped and well staffed referral centre. There is little doubt that the outcome of surgery is dependent on the experience of the surgeon carrying out the procedure.
Surgery involves opening the abdominal cavity, locating the shunting vessel and closing this vessel to re-direct its blood through the liver. In many cases, closure of the vessel must be carried out in a slow and gradual manner. This is generally achieved by the placement of a cellophane band around the vessel. The band causes the gradual closure of the shunting vessel over a four to six week period. This gradual closure allows the previously under-used blood vessels within the liver time to develop without producing an excessively high blood pressure within the portal vein (portal hypertension). Under certain circumstances, other devices or materials may be used to close the shunting vessel. Options include the placement of silk suture or an ameroid constrictor around the vessel (both cause the gradual occlusion of the vessel), or the placement of coils actually inside the vessel itself which then encourage the development of a blood clot that causes the vessel to close.
What is the aftercare following liver shunt surgery?
Pets often remain hospitalised for a few days after the surgical management of a liver shunt. They are nursed very closely in the postoperative period and many may spend some time in the intensive care unit where one-to-one nursing care can be carried out.
When patients go home, instructions are provided to restrict their exercise for the first week or so following surgery. They are routinely keep on medical management (restricted protein diet, lactulose syrup and possibly gut-active antibiotics) for up to six weeks following liver shunt surgery. If a patient remains without any clinical signs the administration of medications is reduced and subsequently stopped.
What is the prognosis (outlook) after surgery?
In the majority of cases, the surgical management of a congenital liver shunt will result in the complete closure of the shunting vessel and the restoration of a normal blood flow to the patient’s liver. Such cases can be expected to lead a normal life, requiring no medication and with a normal life-expectancy.
If you have any queries, please do not hesitate to contact us.
Arranging a referral for your pet
If you would like to refer your pet to see one of our Specialists please visit our Arranging a Referral page.