North Downs Specialist Referrals Chemotherapy in dogs and cats

A guide for owners whose pets are undergoing chemotherapy
Will my pet have a normal life whilst undergoing treatment?
This is probably the most important question of all! The goal of chemotherapy is to extend the life of the patient for as long as possible, without compromising the quality of their life. If you feel at any point this goal is not being achieved, please discuss this with your Specialist at the earliest opportunity. In the majority of cases, the cancers that we treat with chemotherapy are rarely cured but treatment often gives a beloved family member many additional months that they would not have had without treatment
Why do we use chemotherapy in cats and dogs?
Sadly, there are medical conditions that affect our dogs and cats that are best treated using chemotherapy drugs. These include different cancers, as well as some non-cancerous conditions such as IBD (inflammatory bowel disease) and GME (granulomatous meningoencephalitis). Chemotherapy is used in these cases because it achieves control of the disease or control of the symptoms of the disease, and it therefore makes the pet’s life better.
But aren’t there side effects from chemotherapy?
For most cats and dogs receiving chemotherapy, side effects are minimal or absent altogether. In fact, in most instances quality of life is actually improved by chemotherapy as the symptoms associated with the cancer, if there are any, are reduced. This means we expect our patients to be performing normal activities including going for their swim in the sea or climbing the occasional mountain if that is what they usually do. However, there are cases in which the risk of a problem turns into a reality. It is imperative that all owners of patients embarking upon a course or chemotherapy are aware of these risks and feel confident that they can recognise and deal with any problems that should arise.
Does it hurt when chemotherapy is administered?
Chemotherapy is often administered by an intravenous injection or infusion. At North Downs Specialist Referrals all intravenous chemotherapy drugs are carefully administered through catheters placed into veins. As long as the catheter is appropriately placed, the treatment does not hurt at all.
Therefore, if the patient is well-behaved it can be given with them wide awake and simply enjoying a cuddle with their nurse. If treatment is not given properly, some chemotherapy drugs are extremely damaging to the skin and tissues under the skin. Examples include the chemotherapy drugs vincristine, vinblastine and doxorubicin.
Are those the only side effects of chemotherapy in cats and dogs?
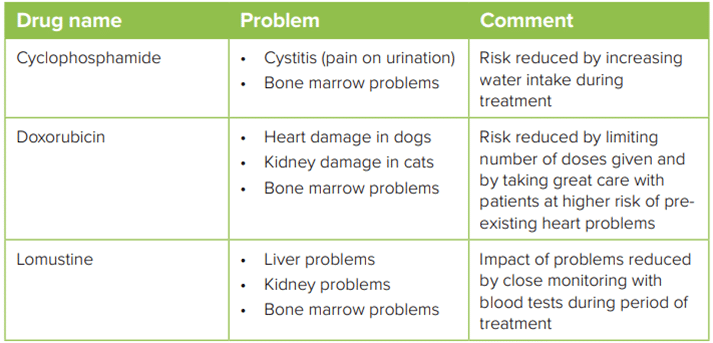
Some chemotherapy drugs also have further specific toxicities. These will be explained to you if your pet receives one of these medications and appropriate steps will be taken to avoid them. A brief summary follows.
Is it safe for me to be around my pet after they have received chemotherapy?
Generally speaking, the risk of a person being exposed to a significant amount of chemotherapy as a result of handling their pet is very low. We do not recommend changing your or your pet’s lifestyle as a result of chemotherapy treatments. This means that they may continue to sleep in your bed, to mix with other household pets, to share a litter tray with other household cats and, unless you are instructed otherwise, to eat their normal breakfast on the morning of their chemotherapy treatments.
However, because repeated, long-term exposure to chemotherapy drugs can result in severe health problems, some precautions are necessary. A small amount of chemotherapy may be excreted in your pet’s urine and faeces for up to 72 hours after a dose of chemotherapy is given. It is important to avoid contact with your pet’s urine or faeces during this time.
- If your pet has an accident in the house, wear gloves when cleaning it up. Wipe up the waste first and then clean the area with a mild soap and water solution three times using disposable paper towels. Place these materials in a plastic bag and dispose of them in an outside/garage waste receptacle.
- In general, for cats change the entire litter tray once daily for the first 2 days after chemotherapy administration and wear disposable gloves when doing so. Be diligent about scooping waste throughout the entire time your cat receives chemotherapy. Dispose of the waste into the toilet or an outside/garage waste receptacle.
- Dogs should urinate or defecate in low-traffic areas (e.g. not in the sandpit where children play, not near the picnic table).
Although exposure of a pet owner to chemotherapy residues from routine handling of their pet is unlikely, certain people are considered at
greater risk if they were to be exposed to chemotherapy. Women who are breastfeeding or pregnant, children, people trying to conceive (both men and women) and immunosuppressed individuals (for example, those receiving transplant medication) should never directly handle chemotherapy drugs or contaminated urine or faeces. In addition, patients should not be allowed to lick their faces. Small children are particularly at risk due to their height and the lack of hygiene awareness.
Are there any special precautions for giving oral chemotherapy drugs to my pet?
Always wear gloves when handling chemotherapy tablets or capsules and wash your hands thoroughly once administration is complete. For dogs, you can put the pills into a ‘meatball’ of tasty food and give the pill before the pet’s meal when they are most hungry. Unfortunately, this does not work for cats and you often have to physically administer the tablet or capsule to them. Please ask your specialist or one of the veterinary nurses for a demonstration of how to administer oral medicine to your pet if you are not sure.
Never split or crush the tablets and do not open the capsules. This allows the chemotherapy drug to become airborne in tiny amounts and can cause you to become exposed. If your pet spits out their medicine and it begins to ‘melt’ or break apart, pick up the medication wearing gloves and using paper towels. Wipe the floor with a diluted soap and water solution three times. Put the paper towels and medication into a plastic bag and dispose of it in in an outside/garage receptacle. Do NOT administer a further dose of medicine as your pet may have absorbed some of the chemotherapy and administration of another pill may cause them to be overdosed. Call your oncologist for advice about what to do next.
Who should not handle chemotherapy intended for administration to pets?
Again, women who are breast feeding or pregnant, children, people trying to conceive (both men and women), and immunosuppressed individuals should never directly handle chemotherapy drugs
Does chemotherapy make pets sick?
Chemotherapy can cause cats and dogs to vomit. This is exceptionally uncommon with most of the chemotherapy agents we use at North Downs Specialist Referrals. If it does happen, it is expected to arise in the first 12 to 72 hours after treatment and is sufficiently short-lived that no treatment is indicated. Remove food for 12-24 hours but offer water frequently to maintain hydration without stimulating further vomiting. If your pet seems depressed or withdrawn, if the vomiting continues for more than 24 hours or contains blood, you should contact your local veterinary surgeon or your oncologist.
In the event that vomiting does occur, we do have very effective treatments for stopping it. These can be provided in advance for administration at home if you are concerned. Sometimes your oncologist will be sufficiently concerned to dispense anti[1]vomiting treatment before chemotherapy is administered. Do please ask if you are worried about this.
Do pets get other intestinal disturbances too?
Diarrhoea rarely occurs and is usually mild and short-lived. Sometimes there is a small amount of blood but the patient is otherwise well. However, if your pet seems depressed or withdrawn or if the diarrhoea continues for more than 24 hours, you should contact your local veterinary surgeon or your oncologist.
It is also possible that a loss of appetite will develop. Tempt them with their favourite foods; warming and moistening the food slightly may improve its palatability. For dogs, adding lean white meat or scrambled eggs can help. Oily fish may tempt cats. If this condition persists for more than a day, medication may be necessary; please discuss this with your veterinary oncologist. In extreme cases, cats can develop anorexia lasting three or more days. This is a severe and unusual manifestation of chemotherapy-associated side effects. Please contact your oncologist If you are concerned about this.
Does chemotherapy cause reduced immunity?
Chemotherapy drugs interfere with the production of white blood cells. This can cause the body’s normal defence mechanisms to fail. Under normal circumstances, the immune system keeps otherwise ‘friendly’ bacteria friendly, by restricting them to where they are supposed to be, mostly in the intestine and definitely not in the blood stream. If this defence barrier fails, bacteria can enter the blood stream; this is septicaemia.
In septicaemia, the patient becomes ill really quickly with signs typically comprising weakness, withdrawal, tiredness, reduced appetite and a very high temperature. If it is left untreated, the condition would be fatal. However, since this almost invariably arises due to transfer of otherwise non-harmful bacteria, there is typically a rapid and complete response to antibiotics. In most cases, the period of risk occurs in the second week after chemotherapy administration.
Always observe your pet closely during treatment and telephone us if you feel they seem ill or you have any questions or concerns. Call us on 01883 741440.
Signs of Septicaemia:
- High temperature of 40°C/104°F or more (rectal temperature is normally 38-39°C/100-102.5°F)
- Marked lethargy or listlessness (reluctance to interact, eat, play)
- Disinterest in food
- Severe vomiting/diarrhoea
There is nothing to stop you taking your dog’s temperature yourself; with cats one would perhaps think twice! This situation can be treated and is almost always successful. However, an extended delay before treatment may result in a severe infection or even death. In the first instance contact your local veterinary practice. However, we will see this type of emergency at any time.
Do not wait overnight if you suspect septicaemia!
Will my pet lose their fur?
- Unlike people receiving chemotherapy, hair loss in cats and dogs is usually very minor
- Cats are expected to shed whiskers over the course of a chemotherapy protocol
- Long-haired dogs are likely to lose their outer coat but not to develop bald patches
- Areas where fur has been clipped for surgery or chemotherapy administration may grow back very slowly
Dog breeds susceptible to hair loss
There are some dog breeds that are more likely to experience hair loss due to chemotherapy.
If you own a Poodle, Old English Sheepdog, Schnauzer, Hungarian Puli, Lhasa Apso, Shih Tzu, Bichon Frise, Yorkshire Terrier, Maltese Terrier, or curly coated terrier such as an Airedale or Welsh Terrier, you should expect that your pet will lose a more significant amount of hair during the initial stages of chemotherapy.
For all pets, the hair that is lost due to chemotherapy will grow back after the course of chemotherapy has been completed or once treatments are given less frequently. Sometimes hair may grow back a slightly different colour.
What happens when treatment is completed?
Once a course of treatment is completed, your Specialist will discuss follow-up appointments for monitoring purposes. Please observe your pet closely during treatment and telephone us if you feel they seem ill or you have any questions or concerns. Your pet may need to be seen by us or your own vet (or their emergency service) if there are any severe side effects.
Arranging a referral for your pet
If you would like to refer your pet to see one of our Specialists please visit our Arranging a Referral page.