
We often receive histopathology reports inviting us to request additional stains or tests. Often, the value of these tests is not clear. The additional tests are often expensive. There can be multiple options for the tests being suggested. And, wasn’t the point of performing the pathology test in the first place to make your decision-making easier, not harder?
So, the question you need to ask (it is the same before running any diagnostic test) is…
Will the result of this test affect a treatment or management decision?
This guide will run through the most common additional tests offered. We hope it will be useful. It will not answer the question in every situation. It is not supposed to replace talking to one of us about a case. We hope you know that we are always happy to take advice requests at any time.
Mast cell tumours
There appear to be an almost limitless number of recommended tests and combinations of tests which can be added to the foot of a histopathology report describing a canine mast cell tumour. Sometimes the recommendations are tailored to the dog’s specific tumour. Sometimes, the same text is copied and pasted to all mast cell tumour reports. If you take a little time to digest the standard information provided in the normal course of things, there are actually remarkably few specific instances where these tests will be useful. First, consider the mast cell tumour grade.
Tumour grade
We would encourage you to think about the result you expect to receive before you open it: will there be clear margins, what do you expect the grade to be? You will be right most of the time! We base a lot of management decisions on the reported grade of the tumour. Dogs with high-grade tumours have an increased chance of metastasis. These dogs should be staged (check regional lymph nodes and abdominal viscera). They are also likely to benefit from chemotherapy or radiotherapy after surgery. These may be cases that need referral to a Specialist.
Dogs with low-grade tumours will often have a great outcome with simple surgery. Those patients have no need for clinical stage evaluations or for follow-up chemotherapy.

Therefore if a tumour looks high-grade (fast growth, oedema, ulceration) and the report says high-grade, we know the dog is likely to need more investigation and treatment. If the tumour looks low-grade and the report shows the tumour is low-grade and completely removed, the dog is likely to need no further treatment.

If the appearance of the tumour and the appearance under the microscope do not match, additional tests can help to decide which one is right and what to do next. Similarly if the tumour is on the borderline between low-grade and high-grade, further tests can also be of use do determine how the tumour is going to behave. In both of these instances, the results of the additional tests will influence your management and therefore are appropriate.
Which test/s?
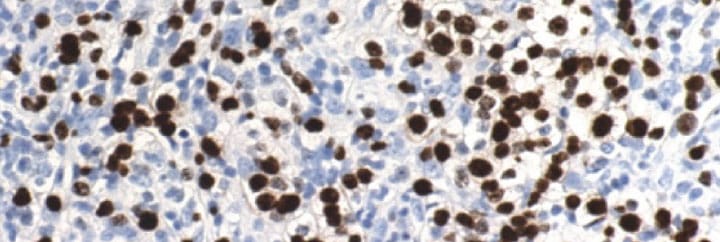
There are a number of available tests and there are lots of combinations of tests. To help you to determine the aggressiveness of the tumour, if that is not already clear from the clinical and histological information you have, the most reliable is the Ki-67 test. This is an immunohistochemical test which identifies proliferating cells under the microscope. Of all the available tests, Ki-67 has the most evidence to support its use in the context in which we are likely to use it, namely, distinguishing more aggressive from less aggressive Patnaik intermediate-grade tumours. Ki-67 has been shown to be more useful than the other proliferation markers, AgNOR and PCNA. Your lab should be able to discuss the interpretation of the Ki-67 test if you run it. Please also feel free to contact us at NDSR.

What about KIT?
We are often asked about whether to run testing for KIT. There are two KIT tests.
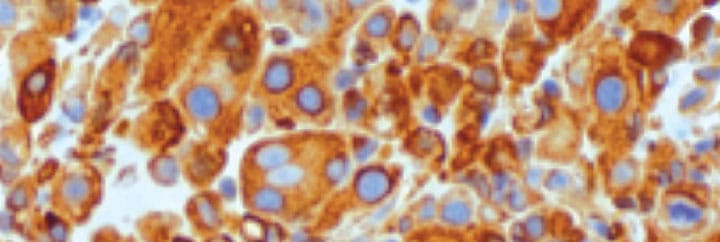
The KIT staining pattern can be used like the Ki-67 test to determine how aggressive a mast cell tumour is. This is scored I, II and III, with III being the most likely to behave like a high-grade tumour. There remains no evidence to date that this test is more reliable than simple histological grade. Some users run this test and Ki-67 together. If there is agreement between the tests, interpretation is simple; if the tests are contradictory, interpretation is challenging.
There is also a PCR test which checks for mutations in the KIT gene. KIT mutations are only present in 30% of tumours. However, they are found more frequently in higher-grade tumours. The reason this test might influence clinical management is that a positive result would justify the decision to use a tyrosine kinase inhibitor. Non-resectable tumours with a KIT mutation have around a 70% chance of responding to Masivet or Palladia and tumours without a mutation have around half this chance. The owner may therefore decide to go for treatment in cases with the mutation or pursue another option (chemotherapy) if the KIT gene is not mutated.
Other tumours: immunohistochemistry
Immunohistochemistry (IHC) involves application of an antibody or mixture of antibodies to a pathology specimen to identify whether a specific target protein is expressed by the cells under investigation. If the target of the antibody is present on the tissue, the antibody will bind it and a fluorescent dye attached to the antibody will be visible under the microscope. If the antigen is not present, there will be no fluorescence. There are antibodies available for a number of different tissues. Some labs perform the stains in-house, others will send them to other pathology centres. This is why it can take anything from a couple of days to a couple of weeks for the results to be returned.
The pathology lab will suggest performing immunohistochemistry in two situations.
To achieve a histopathological diagnosis
Some tumours will be anaplastic; this means that they no longer resemble their tissue of origin and so cannot be recognised by routine histopathology examination. Pathologists will usually have a few tumours in mind and suggest IHC to differentiate between these. Examples include: oral amelanotic melanoma vs. sarcoma, and histiocytic sarcoma vs. lymphoma vs. plasma cell tumour. If the question being asked when taking the biopsy is, “Is this definitely a tumour?“ and the owner is not going to treat it, there is no need to perform the IHC. Most of the time, however, there will be vastly different treatment options for the different diagnostic possibilities. Discriminatory testing is therefore necessary.

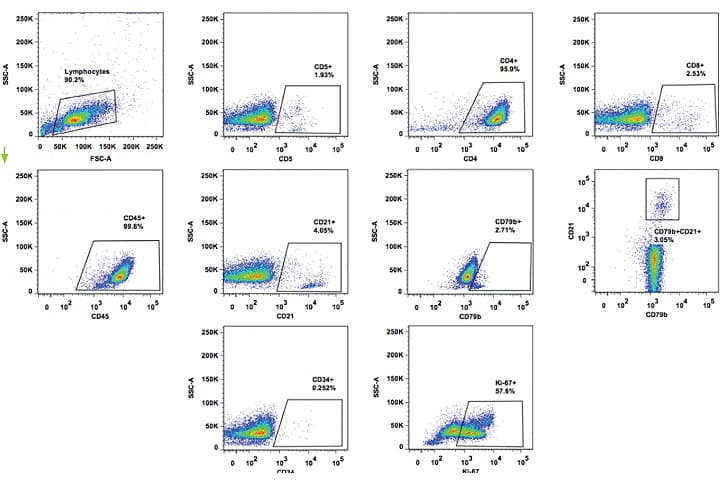
To type a lymphoma
The other main use for IHC is to differentiate between T and B cell lymphomas. At NDSR we are now moving towards recommendation of a more tailored chemotherapy protocol depending on the exact type of lymphoma a dog has. Simple discrimination into broad B and T cell categories is helpful but generally speaking, further information is required. So again, the decision to request the test is defined by the question you are asking at the start. If the owner is going to consider a referral appointment, performing IHC will often simply end up duplicating costs as the same information is gained alongside more detailed analyses of lymphoma type. If the owner is interested in pursuing a chemotherapy protocol solely in first-opinion practice, there are a number of different treatment possibilities and the B/T immunophenotype of lymphoma can change this, so it is often worth knowing.
A very important consideration here is the apparent state of health of the patient at the time of considering requesting IHC. Some lymphoma patients are unwell (we call this substage b). It can take up to two weeks for the results of B/T IHC to be returned, in which time the patient can die or their condition can deteriorate markedly. Under these circumstances, delaying treatment until receipt of an IHC result is definitely not appropriate.
It is worth noting that there other ways of defining the B/T immunophenotype of lymphoma. IHC is what will be suggested if you have biopsied a lymph node. With cytology, the same test can be performed, but it is called immunocytochemistry. PARR can be performed on cytology or histology specimens to diagnose lymphoma, but is arguably not as useful for typing lymphoma.
Flow cytometry can be run on fine needle aspirate samples and is a very useful test for defining lymphoma subtype. However, unlike IHC, the samples need to be sent in a special medium and the test must be performed within 24 hours of sampling. There is not the same requirement for IHC, which is run on formalin-fixed specimens and can be run at any time.
Key messages
- Always ask yourself, ‘Will the result of this test affect a treatment or management decision?’
- Prognostic markers are only useful when the prognosis is not already clear
- Ki-67 is the most reliable discriminatory marker of prognosis in (Patnaik) intermediate-grade mast cell tumours
- Immunohistochemistry for definition of tumour histogenesis is only useful when tissue of origin is not clear and when the diagnoses under consideration would be managed differently
- Do not delay treatment of a systemically unwell lymphoma patient because you wish to wait for B/T immunophenotype results
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Oncology

Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Oncology team.
Advice is freely available, even if the case cannot be referred.
Oncology Team
Our Oncology Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.