
The results of a recent survey amongst North American vets by Reader and Colleagues (2021) highlighted the high prescription frequency of gabapentin (with 69% of participants prescribing it on a daily to weekly basis).
The main reason for gabapentin prescription was as a substitute for NSAIDs in acute pain cases. Furthermore, in the same study only half of the vets knew the exact mechanism of action of gabapentin.
Gabapentin is perceived as a low-risk category for substance abuse in veterinary personnel. Although no surveys have been conducted in the UK, we believe gabapentinoids are currently prescribed very frequently worldwide.
Gabapentin
Gabapentinoids (gabapentin and pregabalin) were developed to treat seizures in humans and subsequently in animals (Platt et al., 2006).
They were later licensed for the treatment of chronic pain syndromes such as postherpetic neuralgia, fibromyalgia and neuropathic pain in humans.
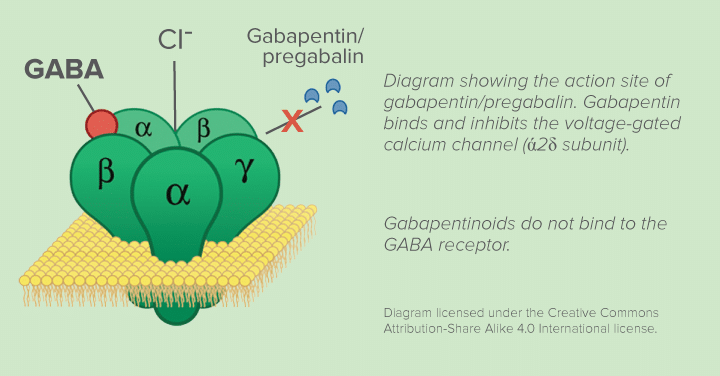
Despite its name, no association was found between higher GABA activity levels after their administration and anti-nociceptive effects.
The mechanism of action of gabapentin includes the inhibition of voltage-gated calcium channel (ά2δ subunit).
This leads to a decrease in release of excitatory mediators from the pre-synaptic membrane.
Furthermore, there is evidence that the ά2δ subunit levels increase in states of hyperalgesia and neuropathic pain models (Maneuf et al., 2006).
Gabapentin as a pre-appointment sedative
Gabapentin can be administered off-license at higher doses to exploit its sedative side effects.
Doses in cats are 50-100mg/cat and 20+mg/kg in dogs (2-3 days before the visit or the night before and the morning of the visit 2-3 hours in advance).
*Be aware no studies have been published in dogs (Erickson et al. 2021)
Current evidence
- Several studies evaluated the clinical effect of gabapentin in dogs and cats with mixed results. It is difficult to compare studies as they used different protocols of administration and doses.
- In a study, gabapentin was administered to dogs undergoing mastectomy and resulted in lower amounts of morphine required in the gabapentin group (Crociolli et al., 2015).
- No additional benefits of administering gabapentin were found in a study evaluating acute pain after forelimb amputation in dogs (Wagner et al., 2010).
- In cats undergoing ovariohysterectomy, no differences were noted when gabapentin was compared with different postoperative analgesic protocols (Steagall et al., 2017).
- The administration of 10mg/kg of gabapentin BID did not result in a reduction in postoperative pain levels in dogs undergoing intravertebral disease surgery (Aghighi et al., 2012).
- Promising results were found in case reports and studies of treatment of trauma-related pain in cats (Lorenz & Comeford, 2013; Vettorato & Corletto, 2011), neuropathic pain, lumbosacral stenosis and Chiari-like malformations in dogs (Cashmore et al., 2009; Giudice et al., 2019; Plessas et al., 2015).
- In cats suffering from osteoarthritis, activity levels were lower when gabapentin was administered with an improvement in owners’ perceptions of previously impaired activities (Guedes et al., 2018).
- One trend emerged from the studies: analgesic efficacy of gabapentin might be improved when administering 10mg/kg up to three times per day are used (in dogs) and in cases of chronic pain especially when neuropathic in origin.
Pregabalin
Compared to gabapentin, pregabalin shows:
- Faster absorption (which happens up to the level of colon)
- Linear pharmacokinetics (non-saturable), which means that the plasma concentration is proportional to the dose administered (which is not true for gabapentin)
- Increased receptor affinity, which leads to lower doses needed when compared to gabapentin
- Terminal half-life of 7 hours (making a twice a day administration possible)
A study in dogs undergoing surgery for intravertebral disc disease and received 4mg/kg of pregabalin twice a day had lower pain scores when compared to dogs that did not receive any (Schmierer et al., 2020).
Another study evaluated the use of pregabalin (5mg/kg BID) in dogs suffering from Chiari-like malformation and showed increased tolerance in thermal and mechanical hyperalgesia and allodynia tests together with an improvement in owner-recorded pain scores (Sanchis-Mora et al., 2019).
Indications and side effects
As seen in the studies presented it seems that:
- Both gabapentin and pregabalin are most effective as treatment of neuropathic chronic pain
- More studies are urgently needed to further clarify whether they can be useful in acute pain
- Both have a liquid formulation that can aid administration in domestic species
- Pregabalin has a higher cost but potential clinical advantages
- Both drugs belong to Schedule 3 of the Controlled Drugs List: it is advisable to prescribe them for 30 days maximum at a time and then re-evaluate the patient. We also recommend a monitoring system to assess gabapentin and pregabalin prescription trends, to minimise the risks of abuse in people
| SIDE EFFECTS | |
| Gabapentin | Pregabalin (reported in people) |
| Sedation | Sedation |
| Ataxia | Dizziness |
| Increased appetite | Nausea |
| Vomiting, drooling (mainly cats) | Ataxia |
| Tremors | Blurred vision |
The Pain Ladder
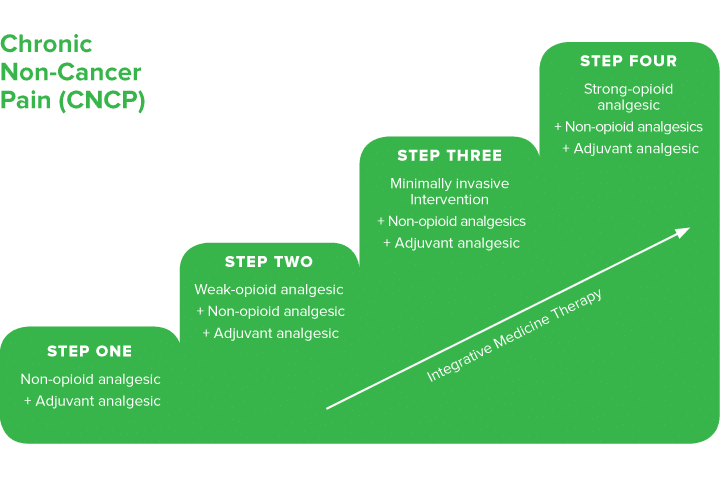
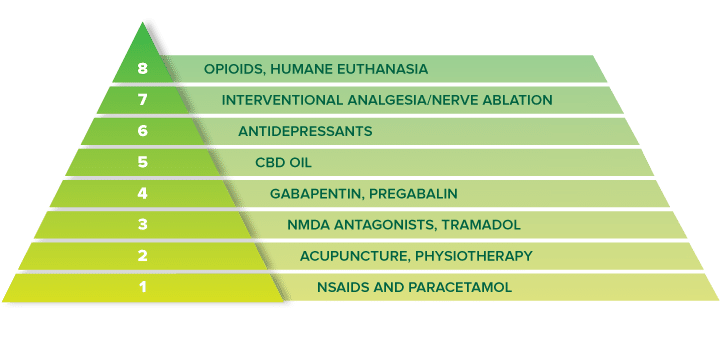
The concept of a pain ladder was introduced by the World Health Organisation (WHO) to guarantee an appropriate selection of analgesics and efficacy (which is reported to reach 80-90% when optimally utilised) (Yang et al., 2020).
The pain ladder is human based but a similar approach could be used in veterinary medicine. The diagram shown is an example of a pain scale adapted to small animals.
As the original pain ladder was designed for cancer pain, here you will find a recent chronic non-cancer pain ladder which also includes adjuvants (acupuncture, CBD oil, physiotherapy) and interventional analgesic procedures.
Quantifying the effects: pain scores
Once we prescribe gabapentin and pregabalin, it’s important to make sure we try to quantify their efficacy over time.
One way to do this is to use one of the chronic pain scales presented on the table that are freely available on the internet. These scales are owner-based questionnaires that can be used to monitor analgesics’ efficacy over time.
Quality of life scores can be considered as well especially when dealing with terminal patients or cancer patients.
| PATIENT | |
| Dog | Cat |
| Chronic Brief Pain Inventory | Feline Musculoskeletal Pain Index |
| Liverpool Osteoarthritis in Dogs (LOAD) | Composite oral/maxillofacial pain scale |
| Helsinki Chronic Pain Index | Client specific outcome measures |
| Vetmetrica | Vetmetrica |
| Canine Osteoarthritis staging tool | Montreal instrument for cat arthritis testing |
| Composite oral/ maxillofacial pain scale | |
Key Points
- It is important to correctly identify the animals in which gabapentinoids might be useful as they are not to be considered substitutes of NSAIDs
- Both gabapentin and pregabalin have shown promising results in neuropathic chronic pain treatment
- Care should be made in animals on long term treatment as both gabapentin and pregabalin are on Schedule 3 of the Controlled Drugs List
- It’s important to try to quantify the effectiveness of gabapentinoids especially when prescribed as a long term treatment
- Overall gabapentinoids are versatile drugs with off label uses that include pre-visit sedation
NDSR Pain Management Clinic
The Pain Clinic delivers an individualised and multi-modal approach to the management of pain. We see a wide range of disorders such as:
- Chronic pain conditions such as osteoarthritis, neck, back and facial pain
- Neuropathic pain
- Cancer pain
- Management of pain and mobility in older patients
- Chronic visceral pain syndrome
If you would like to access this service please call 01883 741449 and ask to speak to the Anaesthesia team.
References:
Aghighi, S.A., Tipold, A., Piechotta, M., Lewczuk, P. and Kästner, S.B., 2012. Assessment of the effects of adjunctive gabapentin on postoperative pain after intervertebral disc surgery in dogs. Veterinary anaesthesia and analgesia, 39(6), pp.636-646.
Cashmore, R.G., Harcourt-Brown, T.R., Freeman, P.M., Jeffery, N.D. and Granger, N., 2009. Clinical diagnosis and treatment of suspected neuropathic pain in three dogs. Australian veterinary journal, 87(1‐2), pp.45-50.
Crociolli, G.C., Cassu, R.N., Barbero, R.C., Rocha, T.I., Gomes, D.R. and Nicácio, G.M., 2015. Gabapentin as an adjuvant for postoperative pain management in dogs undergoing mastectomy. Journal of Veterinary Medical Science, pp.14-0602.
Erickson, A., Harbin, K., MacPherson, J., Rundle, K. and Overall, K.L., 2021. A review of pre-appointment medications to reduce fear and anxiety in dogs and cats at veterinary visits. The Canadian Veterinary Journal, 62(9), p.952.
Giudice, E., Crinò, C., Barillaro, G., Crupi, R., Macrì, F., Viganò, F. and Di Pietro, S., 2019. Clinical findings in degenerative lumbosacral stenosis in ten dogs—A pilot study on the analgesic activity of tramadol and gabapentin. Journal of Veterinary Behavior, 33, pp.7-15.
Guedes, A.G., Meadows, J.M., Pypendop, B.H., Johnson, E.G. and Zaffarano, B., 2018. Assessment of the effects of gabapentin on activity levels and owner-perceived mobility impairment and quality of life in osteoarthritic geriatric cats. Journal of the American Veterinary Medical Association, 253(5), pp.579-585.
Lorenz, N.D., Comerford, E.J. and Iff, I., 2013. Long-term use of gabapentin for musculoskeletal disease and trauma in three cats. Journal of feline medicine and surgery, 15(6), pp.507-512.
Maneuf, Y.P., Luo, Z.D. and Lee, K., 2006, October. α2δ and the mechanism of action of gabapentin in the treatment of pain. In Seminars in cell & developmental biology (Vol. 17, No. 5, pp. 565-570). Academic Press.
Platt, S.R., Adams, V., Garosi, L.S., Abramson, C.J., Penderis, J., De Stefani, A. and Matiasek, L., 2006. Treatment with gabapentin of 11 dogs with refractory idiopathic epilepsy. Veterinary Record, 159(26), pp.881-884.
Plessas, I.N., Volk, H.A., Rusbridge, C., Vanhaesebrouck, A.E. and Jeffery, N.D., 2015. Comparison of gabapentin versus topiramate on clinically affected dogs with Chiari-like malformation and syringomyelia. Veterinary Record, 177(11), pp.288-288.
Reader, R., Olaitan, O. and McCobb, E., 2021. Evaluation of prescribing practices for gabapentin as an analgesic among veterinary professionals. Veterinary Anaesthesia and Analgesia.
Sanchis-Mora, S., Chang, Y., Abeyesinghe, S.M., Fisher, A., Upton, N., Volk, H.A. and Pelligand, L., 2019. Pregabalin for the treatment of syringomyelia-associated neuropathic pain in dogs: A randomised, placebo-controlled, double-masked clinical trial. The Veterinary Journal, 250, pp.55-62.
Schmierer, P.A., Tünsmeyer, J., Tipold, A., Hartnack-Wilhelm, S., Lesczuk, P. and Kästner, S.B., 2020. Randomized controlled trial of pregabalin for analgesia after surgical treatment of intervertebral disc disease in dogs. Veterinary Surgery, 49(5), pp.905-913.
Steagall, P.V., Benito, J., Monteiro, B.P., Doodnaught, G.M., Beauchamp, G. and Evangelista, M.C., 2018. Analgesic effects of gabapentin and buprenorphine in cats undergoing ovariohysterectomy using two pain-scoring systems: a randomized clinical trial. Journal of feline medicine and surgery, 20(8), pp.741-748.
Vettorato, E. and Corletto, F., 2011. Gabapentin as part of multi-modal analgesia in two cats suffering multiple injuries. Veterinary anaesthesia and analgesia, 38(5), pp.518-520.
Wagner, A.E., Mich, P.M., Uhrig, S.R. and Hellyer, P.W., 2010. Clinical evaluation of perioperative administration of gabapentin as an adjunct for postoperative analgesia in dogs undergoing amputation of a forelimb. Journal of the American Veterinary Medical Association, 236(7), pp.751-756.
Yang, J., Bauer, B.A., Wahner-Roedler, D.L., Chon, T.Y. and Xiao, L., 2020. The modified WHO analgesic ladder: is it appropriate for chronic non-cancer pain?. Journal of pain research, 13, p.411.
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Anaesthesia

Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Anaesthesia team.
Advice is freely available, even if the case cannot be referred.
Anaesthesia and Analgesia Team
Our Anaesthesia and Analgesia Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.