
Malignant melanoma is a confusing and challenging condition. Melanoma lesions exhibit a broad spectrum of malignancy from completely benign to disastrously malignant.
Some lesions are easily recognised. But these are typically the less malignant ones. The nasty ones, the ones that will catch you out, are typically less recognisable, often non-pigmented. Inappropriate interventions can then compromise further management, so it pays to have melanoma on your list.
Malignant or non-Malignant Melanoma?
The terminology around melanoma leads to confusion about the real malignancy of melanoma lesions. The terms ‘melanoma’ and malignant melanoma’ are used synonymously in medical and non-medical language in reference to human cutaneous melanoma creating the sense that all melanoma lesions are indeed malignant. Furthermore, the most common manifestation of melanoma in people: UV-induced cutaneous melanoma, is highly malignant. Assumptions are then made that canine cutaneous melanoma lesions are all malignant too. Well, don’t worry.
Most (approx. 70%) canine cutaneous melanoma lesions are non-malignant. They are cured by marginal excision. Physical characteristics that tend to accompany benign behaviour include small size, exophytic nature, verrucose surface and absence of measurable growth. Masses larger than 1cm, dome-shaped masses and masses that bleed spontaneously are likely to be malignant. Following excision, melanomas with a mitotic rate of three (per 10 high power fields) or higher merit further investigation.


Melanoma at oral, subungual and perianal sites should be treated as though malignant. Ocular melanotic lesions in dogs are usually benign.
In cats, melanoma is frequently metastatic at diagnosis. Beware of ocular melanoma as a manifestation of disseminated metastatic disease.
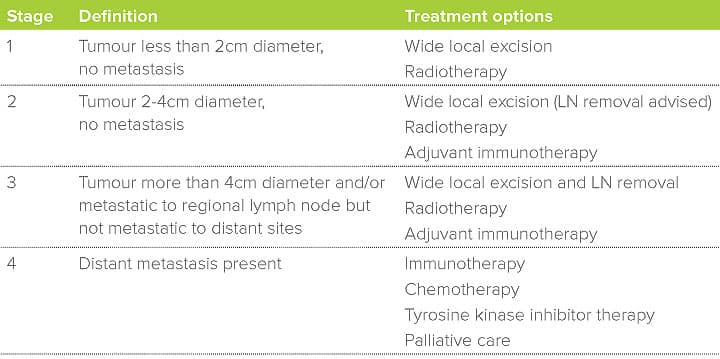
Importance of clinical stage
The most significant determinant of survival in malignant melanoma is the anatomic extent of disease, or clinical stage. Because of the potential for early metastasis, detailed evaluation of the primary tumour site, locoregional lymph nodes and viscera is ideal. Patients with distant metastasis would be unlikely to benefit from surgical intervention. Presence of lymph node metastasis has a significant impact on survival.

In the case of canine oral melanoma, work has been done to assess the suitability of palpation of lymph nodes for determination of metastatic status. Palpation did correctly identify 70% of metastatic cases but it also led to an incorrect assumption of metastasis 40% of the time. Worse than that, palpably normal lymph nodes actually contained metastasis in half of the cases – a coin toss would have been just as reliable! For this reason, we only recognise the results of cytology, or histology to define lymph node metastatic status.
Excision or biopsy?
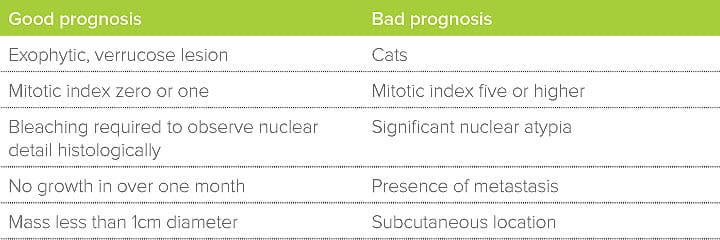
Benign melanocytic lesions will be cured by marginal excision. Malignant melanoma, however, can be notoriously infiltrative. For clear-cut cases, it is easy to make the right surgical decisions. Problems arise when the behaviour of the tumour is not so clear-cut (table 2). Malignant melanoma, particularly oral (mucosal) malignant melanoma, has a nasty habit of developing horizontally along the epithelial basement membrane. This infiltration is utterly undetectable macroscopically but will consistently lead to incomplete excision of even the most innocuous-looking oral melanoma lesions. Revision surgery (not always possible) or radiation therapy is then required to manage residual cancer in the primary tumour site. Prognosis is invariably poorer. For this reason, it is strenuously advised that oral melanomas are only ever diagnosed by incisional biopsy.

Immunotherapy
Melanoma is known to be a strongly immunogenic tumour. This makes it a good target for immunotherapy treatments. These are proving very successful in human patients. In the veterinary world, there is a DNA plasmid vaccine which shows exceptional efficacy when used under optimal conditions. In the first 500 cases to receive this vaccine, after complete removal and/or appropriate radiation therapy of primary tumour and regional lymph nodes, vaccine administration resulted in 57% of cases with stage 3 disease still being alive after three years. This compares to an average life expectancy of only three months before the vaccine was available!

What about proliferation markers?
On receipt of a histology report, you are likely to be invited to request additional histological testing. These tests can be helpful but there are many instances when they are not. As a general rule, proliferation markers are helpful in those situations where a clinician cannot be sure about whether a lesion is at the good end or the bad end of the spectrum. Table 2 lists characteristics which we would consider good enough or bad enough that the degree of malignancy is clear.
Key messages
- In dogs, cutaneous melanoma is usually benign whereas oral and subungual melanoma is usually malignant
- In cats, melanoma is invariably malignant
- In dogs with oral melanoma, normal-sized locoregional lymph nodes contain metastasis 50% of the time
- Marked improvements in survival and quality of life are seen with the appropriate use of a melanoma cancer vaccine
- Optimal control of oral melanoma is severely impaired by incomplete first surgery
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Oncology

Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Oncology team.
Advice is freely available, even if the case cannot be referred.
Oncology Team
Our Oncology Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.