
Tail pull injury is caused by the traction on the tail following a traumatic event. This is a common neurological condition in cats and in most of the cases, is the consequence of a road traffic accident.
Sacrocaudal or intercaudal luxation/fracture, as well as sacral spinal cord segments and cauda equina injury are commonly the consequence of tail pull injury. The neurological signs are mainly related to bladder and anal sphincter dysfunction, making tail pull injury a devastating condition in an otherwise healthy cat.
The traumatic traction of the tail may be associated with sacrocaudal or intercaudal vertebral luxation or in some cases sacral fracture. These lesions may lead to:
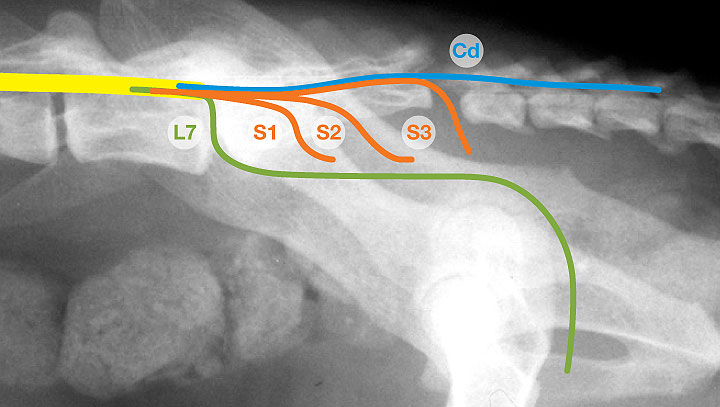
- Sacral and caudal spinal cord segments injury (S1-Cd5)
- Cauda equina and its spinal nerves injury (L7-Cd5)
Common neurological signs are therefore those occurring secondary to impaired neural supply to the PELVIC LIMBS (sciatic nerve), TAIL (caudal nerves), BLADDER (pelvic and pudendal nerves), PERINEUM (pudendal nerve), and ANUS (pelvic and pudendal nerves).
Clinical presentation commonly includes:
- Lumbosacral hyperaesthesia and swelling;
- Pelvic limb paresis, plantigrade stance and weakness;
- Flaccid tail, with/without nociception;
- Urinary incontinence, constantly leaking urine with flaccid bladder often difficult to express;
- Decreased/absent anal tone and perineal reflex
The most severe consequence generally relates to anal sphincters and bladder dysfunction, which makes management of these cases challenging as only a few owners are able and keen to manage a pet with permanent faecal and urinary incontinence
Tips for management of cats with tail pull injury
INITIAL ASSESSMENT
- Patients with tail pull injury should be examined thoroughly, as we should bear in mind that they might have multiple injuries, such as pelvic and femoral fractures, as well as thoracic and abdominal injuries.
- If other injuries are ruled out, neurological examination should focus on pelvic limbs function, motor and sensory function of the tail, assessment of anal tone and reflex as well as perianal sensation.
- Evaluation of the presence of voluntary urination: urine found in a kennel is not indicative of urinary function!
DIAGNOSIS
- The diagnosis of ‘tail pull injury’ is generally obtained by observing sacrocaudal/intercaudal vertebral luxation or sacral fracture on plain radiographs.
- Lateral projection often reveals the lesion; orthogonal views should be added to rule out additional injuries.
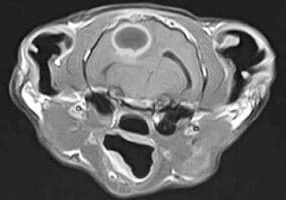
- Further imaging (MRI/CT) is indicated mainly when multiple injuries are suspected and when neurological signs compatible with tail pull injuries are not supported by the radiographic changes.
DIFFERENTIAL DIAGNOSIS
- Main differential diagnosis to consider in animals with neurological signs compatible with tail pull injury are:
- intervertebral disc disease (intervertebral disc extrusion/ protrusion, acute non-compressive nucleus pulposus extrusion);
- fibrocartilagineous embolism;
- discospondylitis/abscessation;
- lymphoma, vertebral tumours.
TREATMENT
- In case of loss of sensory and motor function of the tail, and micturition impairment, treatment mainly consists of medical management:
- patient stabilisation;
- cage rest;
- analgesia;
- detrusor/urethral sphincters pharmacological modulation;
- manual expression of the urinary bladder at least 2-3 times a day. An indwelling urinary catheter can be placed for few days after trauma.
A cystotomy tube could be placed until micturition is restored or for long-term management (useful to assess cat’s urinary function; consider complications).
Tail amputation should be considered to prevent further neurological damage due to traction on nerve roots, to improve return of motor function and to reduce the risk of long-term hyperaesthesia. However, this is generally recommended once urinary function is restored or in conjunction with cystotomy tube placement.
POSSIBLE COMPLICATIONS
- Tail necrosis and self-mutilation
- Faecal incontinence, constipation
- Urinary tract infection: urine should be regularly monitored and treated with antibiotics on the basis of culture and sensitivity testing.
PROGNOSIS
- A valuable test to obtain prognostic information is the evaluation of sensation at the base of the tail (stimulation of the base of the tail by closing forceps across the bones of the tail and assessing any conscious response):
- Intact tail base pain sensation ➔ high likelihood (100%) that the cat will regain ability to urinate within 30 days
- Absent tail base pain sensation ➔ indicates an approximate 40% chance that the cat will not regain ability to urinate within 30 days
- The prognosis for a return to normal pelvic limb function is usually excellent
- How long should we wait for return of urinary function? Ideally allow at least four weeks. However, absence of perineal deep pain perception and areflexic anal sphincter longer than 2 weeks, is suggestive of severe damage and poor prognosis.
Detrusor/urethral sphincters pharmacological modulation
In order to understand the medical management of the bladder, it is important to know its innervation as each nerve will control micturition differently.
The mechanism of micturition is complex and implies the correct functioning of the detrusor muscle and urethra (internal and external sphincters), which act in synergy during the storage (sympathetic nervous system) and voiding (parasympathetic nervous system and voluntary control) phases.
|
Innervation of the bladder | |||
|---|---|---|---|
| Nerves | Spinal cord segment | Nervous system | Function |
| Pelvic n. | S1-S3 | Autonomic – parasympathetic | Detrusor muscle contraction (VOIDING PHASE) |
| Hypogastric n. | L2-4/5 | Autonomic – sympathetic | Detrusor muscle relaxation; Internal sphincter contraction (STORAGE PHASE) |
| Pudendal n. | S1-S3 | Somatic | External sphincter control |
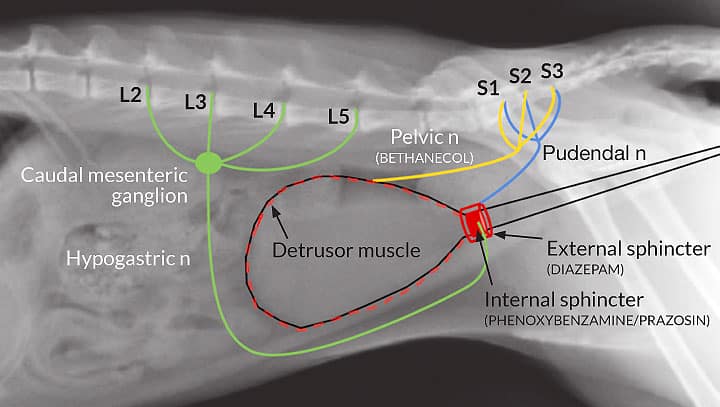
Flaccid bladder with poor detrusor tone due to damage to the pelvic nerve or its sacral segments is often observed in cats with tail pull injury. Instead, the urethral tone may vary, due to the fact that the external urethral sphincter tone is generally lost as a consequence of pudendal nerve lesions, but the internal urethral sphincter tone controlled by the hypogastric nerve is generally intact (reflex dyssynergia). This increased resistance from the internal urethral sphincter, often makes manual expression of the bladder very difficult.
The following drugs are the most commonly used to reduce the urethral tone, facilitate expression of the bladder, and to improve the detrusor muscle tone:
| DIAZEPAM |
Provides relaxation of the external urethral sphincter (generally not needed) Dose: |
| PHENOXYBENZAMINE PRAZOSIN |
Sympatholytic; provide relaxation of the internal urethral sphincter Dose: Dose: |
| BETHANECHOL |
Parasympathomimetic; increases detrusor muscle tone and contractility Dose: |
In cats with micturition disorder, phenoxybenzamine or prazosin can be introduced immediately; bethanechol should not be introduced unless the bladder is easily manually expressed.
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Neurology
Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Neurology team.
Advice is freely available, even if the case cannot be referred.