
Epilepsy is a complex brain disease where sudden and abnormal excessive neuronal activity causes the characteristic transient clinical signs of a seizure.
Recently the International Epilepsy Task Force made a consensus statement on epilepsy and the recommendations are summarised in this article.
How do I know this dog is having seizures?
Always try and get the owner to obtain a video. This can be really useful for differentiating whether it is a seizure despite the owners’ description.
Signs of idiopathic epilepsy
Stereotypical
ie. Each one looks the same
Increased Muscle Tone
Duration
Typically last around 1 minute. Rarely last longer than 5 minutes
Timing
Autonomic Signs
Salivation, urination, defaecation, pupillary dilation
Mentation
Often unresponsive in generalised seizures but can be normal with focal seizures
What is idiopathic epilepsy?
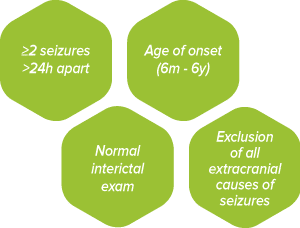
Idiopathic epilepsy is a diagnosis of exclusion and is based on the following:
Pay attention to:
- Proprioception (eg paw placement)
- Menace responses
- Nasal mucosal response
- Mentation
The exact mechanism of why dogs get epilepsy is still poorly understood but we do know that there is some genetic component seen in some breeds of dogs and it can be a result of an ion channel defect, signalling error or other abnormality at a molecular level.
Currently we have causative genes for epilepsy identified in several breeds including the Lagotto Romagnolo who have a juvenile onset epilepsy at several weeks of age and a genetic test for Lafora’s disease in the wirehaired dachshund which causes a myoclonic epilepsy.
Confidence intervals for idiopathic epilepsy:
Tier 1:
- 2 or more seizures >24 hours apart
- Age at onset 6m-6y
- Unremarkable interictal physical & neurological examinations
- Minimum database blood tests & urinalysis
- Complete blood count
- Serum biochemistry profile
- Electrolytes (most importantly sodium)
- ALP, ALT, total Bilirubin
- Urea & creatinine
- Total protein & albumin
- Starved blood glucose
- Cholesterol & triglycerides
- Fasting bile acids
Tier 2:
- All Tier 1 criteria
- Bile-acid stimulation test
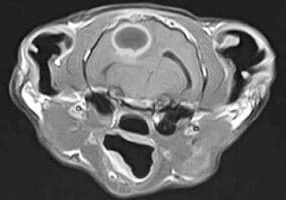
- Unremarkable brain MRI & CSF analysis
Tier 3:
- All above criteria
- Identification of ictal or interictal EEG abnormalities consistent with seizure activity
When to refer for further investigation such as MRI of the brain:
- Age 6y months or >6y
- Interictal abnormalities on neurological examination
- Status epilepticus or cluster seizures
- Drug-resistance with a single anti-epileptic drug titrated to the highest tolerable dose
When to start treatment?
- >2 isolated seizures within 6 months
- Status epilepticus or cluster seizures ( >3 seizures in 24 hours)
- Post ictal signs severe
- Increasing frequency or severity over 3 interictal periods
What is my treatment aim?
Aim for lowest possible concentration associated with >50% reduction in seizure frequency or seizure freedom and absence of intolerable side effects.
Around 20% of dogs will go into remission on anti-epileptic therapy. Labradors appear to have the highest remission rate as a breed (up to 30%).
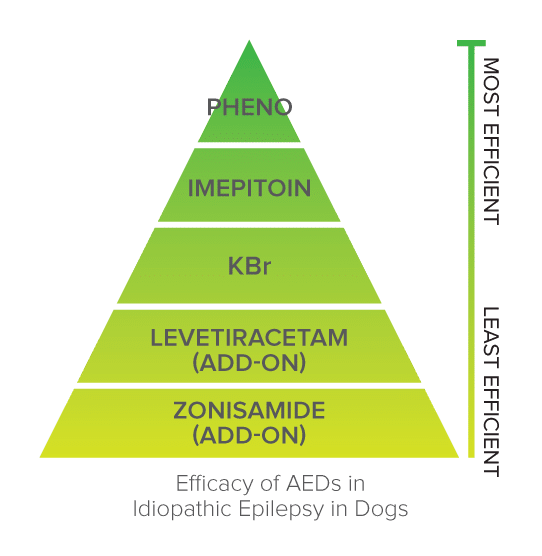
What treatment should I use?
Only phenobarbitone and imepitoin are licensed as first-line treatment of canine IE in the EU.
ALWAYS MAXIMISE SERUM LEVELS OF ONE DRUG BEFORE ADDING ADDITIONAL DRUGS
Phenobarbitone
Can be used as first line monotherapy. It is a GABA agonist (GABA = main inhibitory neurotransmitter). Phenobarbitone (PB) is our most effective AED.
Dosage:
2-4mg/kg PO BID (In animals with status epilepticus or high seizure frequency can load with 15-20mg/kg divided into multiple doses of 3-5mg.kg IV or PO over 24-48h to achieve brain concentration quickly. Serum levels can be measured 1-3 days after loading).
Metabolism:
Hepatic
Serum therapeutic range:
25-35mg/L. If >35mg/L then increased risk of hepatotoxicity.
Adverse effects:
Common = sedation, ataxia, polyphagia, polydipsia; idiosyncratic = hepatotoxicity, haematological abnormalities, necrolytic dermatitis, pancreatitis, dyskinesia, anxiety, hypoabuminaemia.
Test for serum therapeutic levels:
2 weeks after initiation of treatment or change in dosage. Then monitoring every 3-6 months (ideally serum PB levels, CBC, biochemical profile, BAST).
Once steady state has been achieved serum levels can be checked at any time (ie. does not need to be a peak or trough sample).
Lab changes:
Increased serum liver enzyme activities, cholesterol & triglycerides. Thyroid and adrenal testing may be altered. Contraindications: Pregnancy (can be teratogenic), liver disease, dog on medications that inhibit p450 enzymes (e.g. cimetidine, omeprazole, trimethoprim, fluoroquinolones, tetracyclines)
Imepitoin
Can be used as monotherapy. Partial GABA agonist. Only licensed for idiopathic epilepsy with single generalised seizures in dogs (ie. not cluster or focal seizures).
Dosage:
10-30mg/kg PO BID
Metabolism:
Hepatic
Adverse effects:
Common = sedation, ataxia, polyphagia, polydipsia, hyperactivity.
No need for serum therapeutic levels. Ideally CBC & biochemistry every 6 months during treatment (or every 12 months if in remission or has no seizures).
Levetiracetam
Can be used as adjunctive AED. Response rate of 57% in dogs with drug-resistant epilepsy. Also good drug for use in dogs with seizures secondary to structural brain disease.
Dosage:
20-30mg/kg PO TID (may need increased dosing of QID if given alongside PB). Can do pulse dosage for dogs with cluster seizures of 60mg/kg PO after a seizure then 20mg/kg PO TID until seizures do not occur for 48 hours
Metabolism:
Renally excreted unchanged.
Adverse effects:
Behavioural changes, sedation, ataxia, reduced appetite, vomiting
Test for serum therapeutic levels:
No information on therapeutic range in dogs. Can use human range of 12-46ug/L if required.
Gabapentin
Current insufficient evidence for use in dogs of gabapentin as AED.
Dosage:
10-20mg/kg PO TID
Metabolism:
Renal excretion after partial hepatic metabolism.
Adverse effects:
Sedation and ataxia
Potassium Bromide
Not licensed as monotherapy (only as additional AED). Has synergistic effect with phenobarbitone and can improve seizure control in dogs poorly controlled with PB alone.
Dosage:
15mg/kg PO BID (As add on). 20mg/kg PO BID if used as monotherapy. Can also be given once daily in evening but twice daily dosing and administration with food can reduce GI mucosa irritation).
In animals with status epilepticus or high seizure frequency can load with 625mg/kg divided into 8 doses over 48h (should be hospitalised during this). Alternatively for more gradual loading give 125mg/kg/day split into 4 daily doses for 5 consecutive days.
*Need to have constant diet as dietary factors affecting chloride levels can change excretion of the drug**
Metabolism:
Renal (good choice in dogs with hepatic dysfunction). Serum therapeutic range: 1000-2000mg/L (when given alongside PB); 2000-3000mg/L (when given alone).
Adverse effects:
Common = sedation, ataxia, pelvic limb weakness, polyphagia, GI signs (vomiting); uncommon = behaviour change, cough, megaoesophagus, pancreatitis.
Test for serum therapeutic levels:
No information on therapeutic range in dogs. Can use human target range of 12-56ug/L for guidance if really required.
Lab changes:
Elevated serum chloride levels (pseudohyperchloraemia) as assays cannot distinguish between chloride and bromide ions.
Zonisamide
Few published reports on usage (although licensed for canine epilepsy in Japan). Should only be used as AED in dogs poorly controlled on PB, KBR and levetiracetam.
Dosage:
7-10mg/kg PO BID (for dogs on PB).
Metabolism:
Hepatic p450 metabolism.
Adverse effects:
Sedation, ataxia, reduced appetite, vomiting, hepatotoxicity, renal tubular acidosis
Test for serum therapeutic levels:
1 week after initiation of treatment or change in dosage. Human range of 10-40mg/L. CBC & biochemistry every 6 months.
What other treatment options are there?
Diet – Purina® Pro Plan® Veterinary Diets NC NeuroCare™
- Diet rich in Medium Chain Triglycerides (MCT)
- Randomised blinded 6-month crossover trial demonstrated reduction in seizure frequency and severity in dogs on concurrent anti-epileptic treatment
- Designed to be an add-on to treatment rather than a sole therapeutic.
Vagal Nerve Stimulator
- Novel treatment and data in clinical cases is currently lacking although is used in children and has been beneficial in laboratory work on rodents and dogs.
- Surgically implanted generator in the neck sends electrical impulses up the vagus nerve at continuous regular intervals which travel to the brain. This regular stimulation alters the neurotransmitter balance in the brain to inhibit generation and spread of seizures; specifically, it is thought to increase the levels of noradrenaline and serotonin.
- The inhibitory neurotransmitter effect is thought to become more pronounced with prolonged stimulation (over weeks to months) but is also active immediately allowing a magnet to be passed over the device to stop the seizure that is about to start from developing fully.
Can I stop the AED’s if a dog has not had seizures?
- We would only consider this if a dog has been seizure free for 1-2 years
- There is a risk that these dogs start to seizure after withdrawal of the drug and in some cases we can then no longer regain control of the seizures with any medications so this needs to be discussed well with the owners
- We would advise reducing the dosage by 20% or less on a monthly basis if the decision has been made to stop
- If a dog has life-threatening adverse side effects then instant cessation under 24h observation is necessary. Loading with an alternative AED such as KBr or levetiracetam should be initiated promptly.
Key Points
- Suspect idiopathic epilepsy if dog aged 6m-6y at onset of seizures and normal neurological exam and bloods
- Always remember to run a bile-acid stimulation test alongside initial bloods to rule out extra-cranial causes of seizures.
- Always maximise serum levels of one drug before considering addition of another
- Imepitoin is not licensed for focal or cluster seizures. Phenobarbitone should be used in these cases.
- If phenobarbitone is at adequate serum levels and seizure control is not adequate consider levetiracetam or potassium bromide.
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Neurology
Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Neurology team.
Advice is freely available, even if the case cannot be referred.
Neurology Team
Our Neurology Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.