
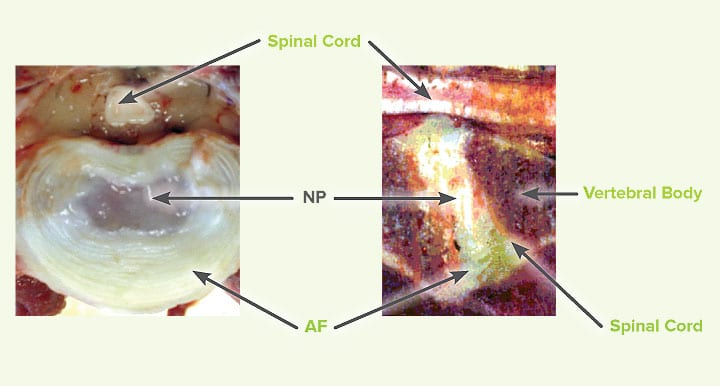
The intervertebral disc (IVD) is an important structure within the spine. The functions are to offer stability and absorb shock during movement such as running, jumping or minor trauma. The structure of the IVD compromises the annulus, the nucleus pulposus and vertebral endplates.
The nucleus pulposus is located in the intervertebral disc space formed by the annulus and endplates. It is the largest avascular structure in the body; its health depends on the nutrients and oxygen coming from the endplates.
The nucleus pulposus function of absorbing shock is possible due to its matrix composition rich in proteoglycans containing sulphate molecules and collagen. The sulphated molecules, attached to the proteoglycan have a great affinity to water which they bind and keep the nucleus well hydrated. The water disperses during the loading phase of the disc allowing the deformation and adsorbing the shock.
The hydration of the nucleus pulposus produces enough pressure to keep the disc well separated.
Degeneration
The first step of IVD disease (IVDD) is the degeneration of the nucleus pulposus. The normal matrix composition is altered, the proteoglycans and collagen composition changes and the hydration lost. In some breeds of dogs such as chondrodystrophoid dogs (i.e. Dachshund, Shih-Tzu, Beagle etc.) this process starts a few months after the dog’s birth. Genes appear to be associated with selection for chondrodystrophic phenotype. The degeneration or dehydration of the nucleus pulposus might never cause problems. The IVDD can progress to more serious problems which cause intervertebral disc herniation. In simple terms the herniation of the disc occurs due to weakening and rupture of the annulus, the nucleus pulposus escapes and impacts the spinal cord. In some cases, trauma might have a role in the intervertebral disc extrusion. The current classification of IVDD includes
- Acute non-compressive disc extrusion
- Acute hydrate intervertebral disc extrusion
- Intervertebral disc herniation Hansen Type 1
- Intervertebral disc herniation Hansen Type 2
Acute non-compressive disc extrusion
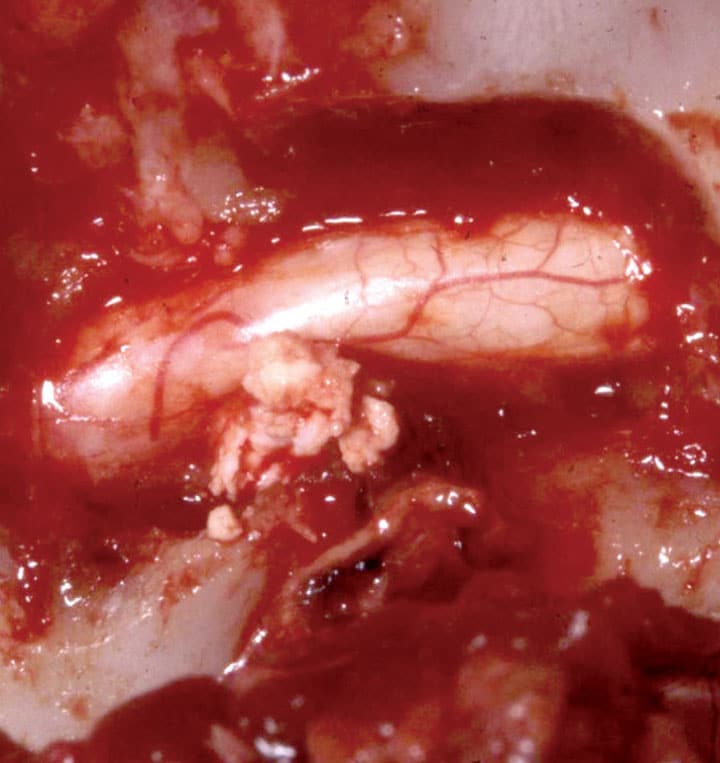
Occurs without previous degenerative process of the nucleus pulposus. A per-acute extrusion of apparently normal IVD nucleus is presumed to be associated with supra-physiological, mechanical stress during athletic activity. A portion of the nucleus is explosively expelled through the annulus with great force, causing a focal contusive injury to the adjacent spinal cord. As the extradural material is non-degenerate and, therefore, highly hydrated, it typically rapidly dissipates or is resorbed, leaving minimal to no spinal cord compression. This type of disc extrusion is referred as ‘acute non-compressive disc extrusion’. See Figure 1
Hydrated nucleus pulposus extrusion
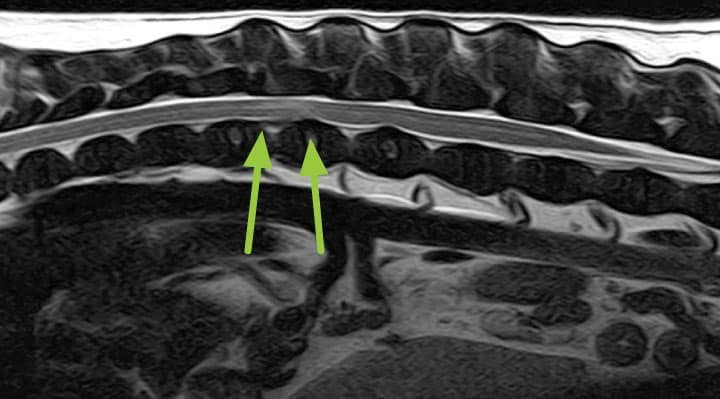
Similar to acute non-compressive disc extrusion; but distinctly different, in which material appearing hyperintense on T2W MRI scans is observed ventral to the spinal cord. These lesions have been described in the cervical region of dogs.
Hansen Type I
Hansen described the pathological features of IVDD in dogs 60 years ago. This extrusion can occur in any direction, but frequently is dorsally directed. Hansen associated this type of degeneration with chondrodystrophic dogs and defined the subsequent nuclear herniation as ‘type I’ IVDD.
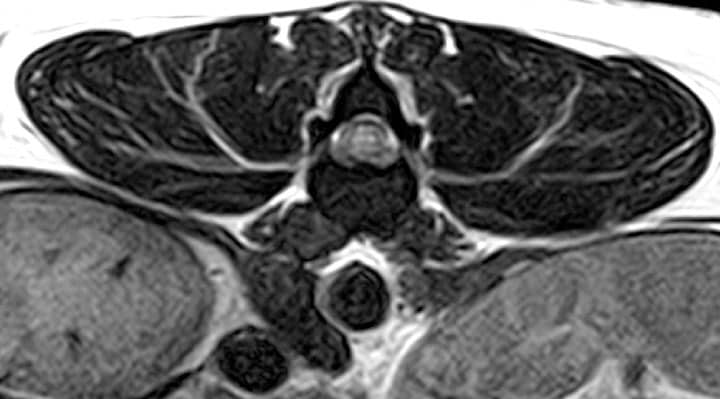
Hansen Type II
This type of herniation is also known as bulging disc. More recent histologic analysis, although generally supportive of Hansen’s original descriptions, has suggested that there is less difference between degeneration in chondrodystrophic and non-chondrodystrophic dogs than was previously assumed. This degenerative process causes thickening of the annulus, especially dorsally.
This can cause the annulus to protrude into the vertebral canal.
Clinical signs
The clinical common denominators of intervertebral disc herniation are spinal pain and paresis or paralysis; importantly, these are not pathognomonic clinical features of IVDD. The onset and severity depends on the speed of herniation, the amount of nucleus pulpous herniated and associated damage to the adjacent vascular structures. Acute non-compressive disc extrusion, hydrated Intervertebral disc and Hansen Type 1 are generally peracute or acute and occur within seconds to hours. The cascade of events that occur following the spinal cord trauma are responsible for further damage of the spinal cord which lead to myelomalacia (softening or liquefaction of the spinal cord).
Pain is often the first clinical sign seen in Hansen Type 1 and this is likely to be due to the stretch and damage of the dorsal longitudinal ligament. As the herniation progresses to affect the adjacent neural structures, meningeal and nerve root compression occur causing further pain and neurological dysfunction.
The degree of spinal cord dysfunction is variable and several classifications for thoracolumbar intervertebral disc herniation have been suggested. The most widely used is a grading from 0 to 5
0 Normal
1 Pain only
2 Pain, ataxia and paresis
3 Pain, ataxia and non-ambulatory paraparesis
4 Pain, paraplegia and urinary incontinence
5 Paraplegia, loss of deep pain and urinary incontinence
This classification is useful to formulate the prognosis, which varies with the severity of the clinical signs. In grade 1-3 the prognosis is in general favourable, grade 4 fair to severe, grade 5 the prognosis is poor. Another poor prognostic factor is the localisation; Lesions at L4-S3 spinal cord segments are likely to cause damage to the lower motor neurons and permanent neurological dysfunction.
Investigations:
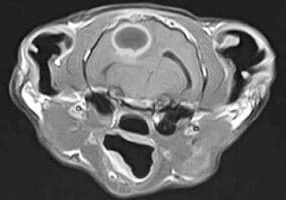
Magnetic resonance imaging (MRI) is considered the gold standard investigation for spinal cord diseases. Computed tomography with or without myelography is another modality which obtains similar diagnostic results to MRI. However, myelography increases the risk of complications. Radiography alone is not a suitable diagnostic modality in IVDD.
MRI is a superior method of investigation for the nervous system due the ability to see the subarachnoid space, spinal cord and soft tissue structure without the use of contrast medium. The extruded disc material and its hydration can be easily identified.
Radiographs can visualise calcified discs within the intervertebral disc space and in some rare cases, within the vertebral canal. The calcified discs within the intervertebral disc space are not the cause of spinal cord dysfunction or pain.

Treatment
In all types of intervertebral disc herniation the treatment protocols should include pain control, cage rest, and anti-inflammatory drugs, careful nursing care for the bladder management, comfort, hydration and nutrition. The use of steroids should be avoided.
Surgical spinal cord decompression has attracted some controversy. It has been observed that in some cases the clinical signs improve in time without surgery.
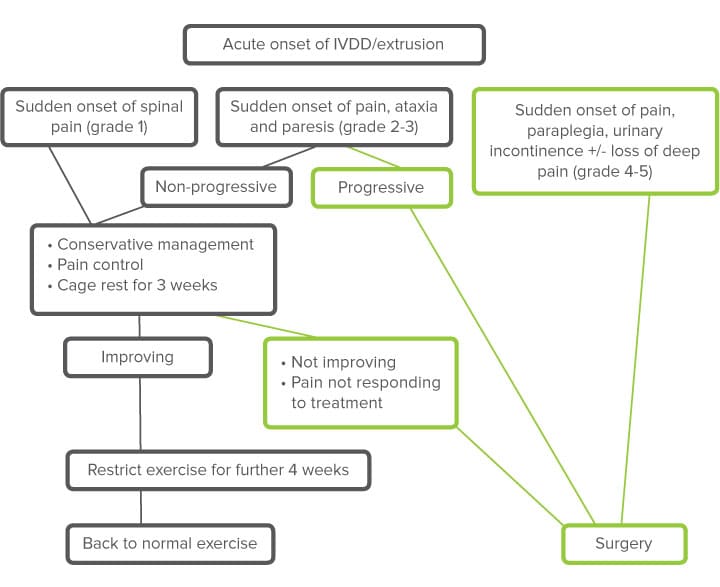
Our recommendation is to perform surgery in severe cases, with a history of progression and lack of improvement with conservative management. Less severe cases can be managed conservatively with cage rest and NSAIDs.
IVDD Key points
- Acute intervertebral disc extrusion occurs in all breeds, but more frequently in chondrodystrophoid dogs
- Plain radiographs do not provide adequate information
- MRI is the superior modality for investigations of spinal cord diseases
- First 2 actions in all acute intervertebral disc diseases are:
- Restrict movement (cage rest)
- Pain management
- Surgery should be considered for grade 4-5 and history of progressive clinical signs
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Neurology
Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Neurology team.
Advice is freely available, even if the case cannot be referred.
Neurology Team
Our Neurology Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.