
Blunt head trauma is common in small animals with up to 50% of the cases due to road traffic accidents.
Patients presenting with head trauma usually will have concomitant injuries, therefore it is very important to perform survey X-rays of the chest abdomen and spine to check for life-threatening conditions such as pneumothorax or haemo/uroabdomen.
Although not all patients with head trauma will have traumatic brain injury, neurological assessment of all polytraumatised patients and prevention of secondary brain injury are mandatory to ensure the best possible outcomes.
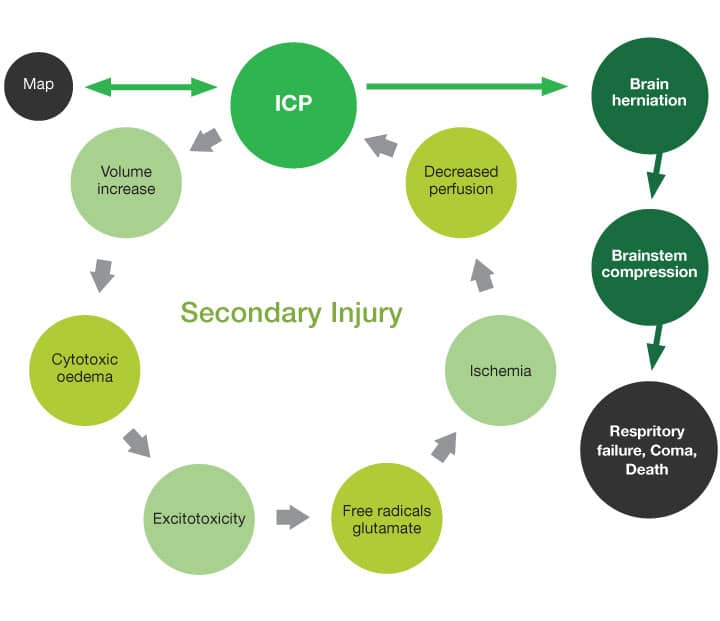
Brain Perfusion and Autoregulation
Cerebral perfusion (and therefore oxygenation) depends directly on arterial blood pressure and intracranial pressure.
CPP = MAP – ICP
After brain trauma, brain autoregulation is lost, and systemic changes in the blood pressure will affect intracranial pressure (ICP) directly. Increases in ICP will lead to:
- Decreased perfusion: leading to ischemia and neuronal death
- Increase in intracranial volume: leading to brain herniation
- Brain oedema: leading to further increases in ICP
Modified Glasgow Coma Score Scale (MGCSS)
It is the best monitor tool, and directly related to survival. Serial neurological examination, as close as every 15 to 30 minutes initially are the key to detect deterioration early.
The MGCSS is based on 18 points, divided in 3 categories, where the maximal punctuation for a category is 6 (normal function).
- Motor function 1-6
- Brainstem reflexes 1-6
- Consciousness 1-6
MGCS > 14 carries good prognosis
A MGCS of 8 correlates with 50% survival
Signs of catastrophic brain herniation include a drop in the MGCS, loss of consciousness, PLRs, and altered cardiac and respiratory patters, such as Cushing reflex, defined by increased blood pressure with bradycardia.
Clinical management
Reduce secondary injury:
- Maintain the head elevated 30° angle
- Do not compress jugulars
- Avoid stress and treat pain
- Avoid coughing on intubation
- Treat seizures when present and provide antiepileptic treatment
- Avoid steroids as they increase the risk of death
Maintain cerebral perfusion and reduce ischemia:
- Correct hypovolemia with crystalloid isotonic fluids, aiming for normovolemia and normotension
- Consider hyperosmotic agents to increase cerebral perfusion and reduce oedema formation
Hypertonic Saline 7.5%
- 4ml/kg over 8 minutes
- Improves systemic blood pressure, cardiac output and cerebral blood flow
- Decreases brain excitotoxicity, modulates neuroinflammation
- Effect lasts 15-75 minutes
- Can cause dehydration, hypernatremia, worsen pulmonary contusions/oedema
Mannitol
- 0.25g – 1g/kg over 20 minutes
- It is also a free radical scavenger
- Takes 15-30 minutes to effect
- Lasts 2 – 5 hours
- Can cause dehydration
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Neurology
Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Neurology team.
Advice is freely available, even if the case cannot be referred.
Neurology Team
Our Neurology Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.