
Hypersomatotropism (HS) is the excessive production of growth hormone (GH) by the pituitary gland.
Acromegaly is the clinical syndrome which results from this, with the classic broad facial features, prognathia inferior, snoring and stertor (due to excess tissue growth in the airways), myocardial thickening and large paws. Hypersomatotropism is the preferred term for this disease as GH excess is often present for a long time before clinical acromegalic features are noted.
How common is feline hypersomatotropism and which cats should be tested?
A large screening study of 1221 diabetic cats found 25% had HS. Most of these cats did not display the typical phenotypic appearance expected of acromegaly. Therefore it is advised that all newly diagnosed diabetic cats are screened for this condition. Some cats with HS have no clinical signs, and can occasionally appear sensitive to insulin treatment initially. However, over time their diabetes will become more difficult to control.
How do I test for hypersomatotropism?
A serum IGF-1 level > 1000 ng/ml has a positive predictive value of 95% for HS. It is suggested that the test is more specific (positives can be believed) than sensitive (a negative result does not rule it out). If you obtain a result of 800-1000 ng/ml and remain suspicious, then retesting later is advised. Insulin requires to be present for IGF-1 to be produced by the liver, therefore it is advised that serum IGF-1 is assessed once a newly diagnosed diabetic cat has been on insulin for 2 months, to reduce the risk of a false negative result.
Further investigations to perform if hypersomatotropism is confirmed
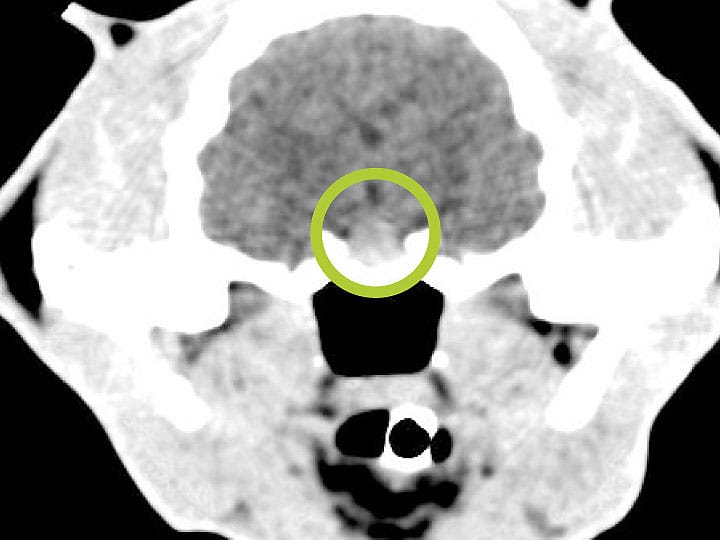
Imaging of the pituitary gland should be performed. MRI is preferred as it is more sensitive for detecting pituitary enlargement or irregularities, however contrast-enhanced CT is a commonly used alternative (due to availability and reduced cost). There is a gradual progression from microscopic pituitary hyperplasia to a macroscopic adenoma (or rarely carcinoma), therefore negative intracranial imaging findings are more likely early in the disease.
Can a cat have hypersomatotropism but not diabetes mellitus?
This has been reported in a small number of cats. It may be identified if IGF-1 is measured in cats that are non-diabetic but have conditions that could be triggered by HS e.g. myocardial thickening, or adult onset snoring and stertor. These cats may or may not eventually develop DM.
What treatment options can be offered?
Hypophysectomy: This removes the tumour and treats the underlying cause. IGF-1 is normalised and 70-92% of cats achieve diabetic remission. However it is only available at a few referral institutions, it is costly, and cats will need lifelong hormone supplementation with levothyroxine, hydrocortisone and DDAVP (+/- insulin). The peri-operative mortality rate is 10%, with a subsequent median survival time of 2.3 years.
Radiotherapy: This can reduce tumour size with little associated morbidity and mortality (but does require multiple anaesthetics). It may be appropriate for cats that are not candidates for surgery (based on owner choice, large pituitary mass or comorbidities). However IGF-1 levels are not expected to be effectively reduced, therefore recurrence is relatively frequent and diabetic remission rates (32%) are lower than with hypophysectomy.
Medical management with insulin alone: If owners decline the above treatments, insulin therapy can be trialled. Some cats will need large insulin doses to manage their clinical signs, therefore there is concern regarding iatrogenic hypoglycaemic events if pulsatile GH concentrations fall low. Owners must be counselled on monitoring for this and also for the risk of developing congestive cardiac failure secondary to myocardial hypertrophy.
Pasireotide: This is a novel somatostatin receptor (SSTR) analogue which decreases IGF-1 levels and has shown potential as a long-term management option for cats with HS. It was administered monthly by subcutaneous injection to cats. Although IGF-1 concentrations and insulin doses were significantly reduced, only 3/7 cats completing the trial achieved remission and some developed diarrhoea. This medication may prove to be too expensive for clinical use and further work is need to optimise dose, efficacy and reduce side effects.
References and further reading:
- Niessen et al. Studying cat diabetes: beware of the acromegalic imposter. PLOS One (2015)
- Fletcher et al. Hypersomatotropism in 3 cats without concurrent diabetes mellitus. JVIM (2016)
- Feldman et al. Feline Endocrinology. Published by Edra (2019)
- Pasireotide long-acting release treatment for diabetic cats with underlying hypersomatotropism. JVIM (2017)
- Van Bokhorst et al. Evaluation of hypophysectomy for treatment of hypersomatotropism in 25 cats. JVIM (2021)
- Fenn et al. Efficacy of hypophysectomy for the treatment of hypersomatotropism‐induced diabetes mellitus in 68 cats. JVIM (2021)
- Wormhoudt et al. Stereotactic radiation therapy for the treatment of functional pituitary adenomas associated with feline acromegaly. JIVM (2018)
Case Advice or Arranging a Referral
If you are a veterinary professional and would like to discuss a case with one of our team, or require pre-referral advice about a patient, please call 01883 741449. Alternatively, to refer a case, please use the online referral form
About The Discipline
Internal Medicine

Need case advice or have any questions?
If you have any questions or would like advice on a case please call our dedicated vet line on 01883 741449 and ask to speak to one of our Internal Medicine team.
Advice is freely available, even if the case cannot be referred.
Internal Medicine Team
Our Internal Medicine Team offer a caring, multi-disciplinary approach to all medical and surgical conditions.